For women, your pelvic floor includes three main organs: the uterus (stores eggs for reproduction); bladder (stores urine before peeing); and the rectum (stores feces before elimination). Normally, these organs are supported by pelvic floor muscles that act as a hammock to ensure they maintain proper function.
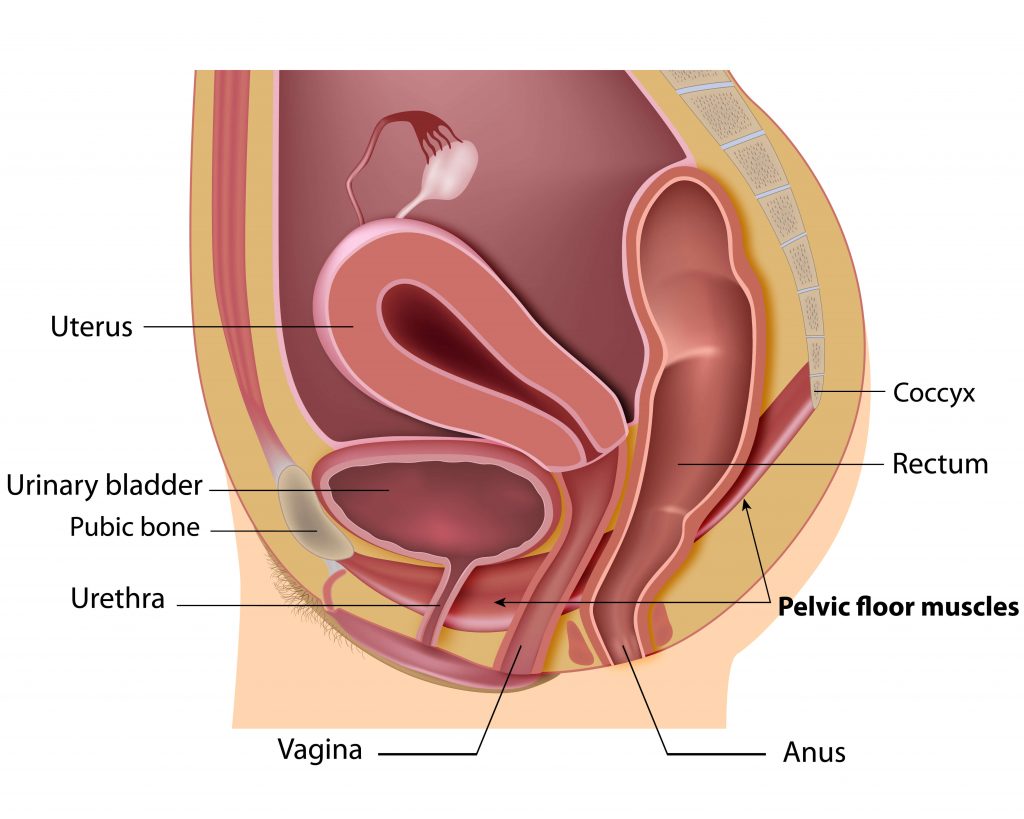
Pelvic floor muscles form this “hammock” by attaching from your pubic bone, which is where your left and right hip bone connect near your genitals, to your tailbone1. These muscles are the bottom portion of your “core muscles”, the muscles that facilitate balance and stability.
This hammock must be kept taught to keep all the organs in place. If the muscles are not strong enough to do their job, your pelvic floor will droop, and the organs will work inefficiently.
Think of your bladder as a water bottle. It needs to be held upright vs on its side to allow for the water to pour out properly. Something must keep it aligned in place to allow for proper flow. When these organs slip out of alignment this is known as a pelvic organ prolapse (POP). POP affects half of all women in the US2, but with proper prevention this number can go down significantly.
Three Biggest Risk Factors for POP
Age. The likelihood of POP tends to increase as you get older, approximately 37% of women affected are between 60 and 79 years old, this number increases to 50% for women who are 80 or older3.
Pregnancy. While age increases the risk, pregnancy is the most common risk factor. This typically occurs several years after childbirth and most likely from a vaginal childbirth (vs C-section).45
Weight. A higher body mass index (BMI) also increases the risk for POP5 due to long-term pressure on your abdomen4. While gaining weight may create the problem, unfortunately, losing weight is not considered an effective way to reverse it6.
While age is unavoidable, and pregnancy is common for the majority of women (86%)7, BMI is the most controllable risk factor. But, the reality is that 66%8 of women are overweight or obese, so at some point, we will all experience some risk factor. We all need to add to our toolkit to prevent and delay weakening pelvic floor muscles.
This prevention comes from training and exercising our pelvic muscles, but the best news is that these are exercises you can do completely while laying down and never breaking a sweat!
Training Your Pelvic Floor Muscles
These muscles are like most of the muscles in your body, they can become stronger through strength training or “resistance” training to improve the symptoms of POP and slow it’s progression. Most women do not think about these muscles until they are not working properly, but the earlier you focus on them the better, because prolapse itself cannot be reversed. It is best to adopt an exercise regimen early and stick with it. Otherwise, POP will occur, impacting your physical discomfort, sex life, body image, and your quality of life910.
This type of muscle conditioning is commonly referred to as” Doing Your Kegels”. Named after Dr Arnold Kegel, an American Gynecologist. Dr Kegel identified the effects of childbirth on these muscles and theorized, and went on to prove through clinical trials, that they could be strengthened, reversing some of the common symptoms.
Kegel developed a device called the perineometer. This device measures how strong you can voluntary contract your pelvic floor muscles by collecting the air pressure in the vagina when a patient is asked to squeeze her muscles as much as possible. This device could determine how weak the muscles are, to see if the patient would benefit from Kegel exercises11.
He observed that women who consistently performed movements to their pelvic muscles would see benefits in only 2-4 weeks. Not only would their incontinence be improved over time, but also intensity and frequency of their orgasms; a side effect he had not anticipated.
Now that we have your attention, what are these exercises and how soon can we do them?!
First, let’s start by identifying the muscles. A simple way to do this is to imagine you are trying to prevent yourself from passing gas. The muscles you would clinch to stop that from happening should have a pulling sensation, those are the muscles you are going to be working on. Another way is to place a finger inside your vagina as if you wanted to stop yourself from urinating. Then try to squeeze your muscles around your finger. The muscles that contract during this are ones that you will exercise during Kegel exercises.
Many women may be surprised that they actually have muscles down there because they have never done these muscular contractions voluntarily. Now that you are aware of what to focus on, you are ready to train yourself and improve your pelvic floor strength.
Performing Kegel Exercises12
Start by lying on your back with your knees bent and feet flat on the floor. Place one hand on your chest and the other hand on your abdomen.
- Step 1. Contract your pelvic floor muscles, this will be that pulling sensation. Hold for 3 seconds.
- Step 2: Release the muscles. Relax for 3 seconds.
Repeat the contract/relax cycle 10 times to complete one set.
This reads as if it too easy to be effective, but in order to do this effectively holding and relaxing your pelvic floor muscles, and only your pelvic floor muscles will require discipline.
Maximize Your Exercises
A common mistake many women make is not fully relaxing between contractions. Your muscles require a full range of contraction and relaxation. If the muscles do not have an opportunity to properly relax, they can become tight. If your muscles become too tight you will have to perform a different set up exercises to address hypertonic (excessive toning) muscles13.
You want to make sure you are only working your pelvic floor muscles and not your abs, legs or buttocks. You can use your hand that’s on your stomach to ensure other muscles are not moving and that your pelvis is not lifting from the ground. Also, you should be breathing out, not holding your breath.
Over time, you will want to increase the duration of your Kegels. Breakup how often you do these sets, not all at once, but build your way up to 30-40 Kegels a day holding them for 10-second contractions and releases. Increase your numbers and duration gradually, 4-seconds then 5-seconds holds until you build up to 10-seconds.
Even though you build up your endurance, throw in a few second holds and releases to mix things up and flex your muscles differently.
Once you get used to these movements, you can start practicing them sitting down and standing up. You can get your 30-40 Kegels in while waiting in lines or traffic. You won’t be bored on a Zoom Call ever again!
Most women say they notice a difference after 4-6 weeks14 and some of those with incontinence may even see less urine leakage with in 12 weeks after starting their routine. The key is consistency and starting NOW. It is much easier to use these exercises to prevent or delay prolapse, than repair it15.
It is also important not to overdo these exercises, you could create problems with urination or bowel movements. Do 3 to 4 sets of 10 Kegels, not 40 at one time.
Kegels to the Rescue
You may have already experience certain activities that trigger leakage. Doing Kegels before doing those activities, such as bending or lifting, may offer some prevention, allowing you to perform those actions without incident. Kegels may also offer you some control in the event you have a sudden urge to pee and are worried you won’t make it to the restroom in time16.
Health Care Professional Kegel Assistance
If you have trouble doing Kegel exercises or would like to increase the effectiveness of your training, here some additional options for you to consider:
Biofeedback Training. Performed by a Physician or a nurse, this training allows the patient to be guided through Kegel exercises. Sensors may be placed on your stomach and inside your pelvic cavity to measure electrical activity. The clinician will receive immediate feedback from those sensors, so you will be corrected on how these movements should be made, allowing you to go home and perform them properly.
Electrical Stimulation. A physician or nurse inserts a tiny probe, the size of a tampon, into your vagina. This probe creates a low-grade electrical current that induces an involuntary contraction to reproduce the muscular response similar to Kegels.
Over the Counter Kegel Assistance
If you need some assistance or want to elevate your training but want to avoid going to a physician’s office, there are some devices you can buy for home, usually under $200.
Here are a few.
Elvie Pelvic Floor Trainer: This device was popularized by Gwynteh Patrow a few years ago. This silicone device is used in five-minute sessions. Its sensors measure force and motion to determine how your pelvic floor muscles are moving. Data is collected on an app so you can measure your progress.
YarLap: This FDA cleared devices uses electrostimulation, similar to what a clinician might do, to stimulate your muscles to contract on their own. You can do this at your own home in 20-minute sessions to improve your strength over time.
Intimina: This is placed inside your vagina and guides you through subtle vibrations to let you know when to squeeze and release your muscles. The device calculates your strength and endurance and increases intensity as you progress.
Kegel weights. There are many options of weights, the most important thing to remember is to find body-safe silicone that avoids degrading over time and bacterial growth as you continue to use it. Weights come in variations to allow you to progress, increasing your weight as you strengthen your muscles over time.
Now, drop to the floor and give me 10! No matter what your age, you can start exercising today, unless you aware of any damage to your pelvic floor muscles that should prevent you from exercising them. If you have any concerns, contact your primary care physician. The sooner you start a plan the longer you can delay and possibly prevent prolapse and reduce the chances of physical discomfort and incontinence, while maybe improving your sex life.
















