Pelvic organ prolapse, or POP, is a very common condition that affects about 50% of women in the U.S. 1 and up to 70% of women wear tampons at least some of the time. 2 So naturally, pelvic health specialists field lots of questions about tampons and POP!
In this article, we’ll briefly explain POP, and then answer some of your FAQs about POP and tampon use.
What is POP?
Pelvic organ prolapse is a pelvic floor disorder in which the uterus, bladder, or rectum (or other tissues and organs) drop from their normal position into or out of your vagina or anus. It can cause physical discomfort and/or impact your sex life, body image, and quality of life. POP can cause bladder leakage as well as other issues.
For some women, there may be no symptoms of POP, and non-invasive interventions, like lifestyle changes, physical therapy, and pelvic floor exercises can really help. Research has proven that pelvic floor exercises help keep pelvic floor muscles “fit,” and can be used as an effective treatment for women suffering with stress urinary incontinence.
Whether you have a prolapsed uterus or simply want to strengthen your pelvic floor muscles, you need to be sure you’re doing Kegel exercises properly. You can use a tool like the INNOVO Urinary Incontinence Kit, which helps you perform Kegel exercises properly, in short 30-minute sessions. Severe pelvic organ prolapse may require surgery.
All About Pelvic Organ Prolapse
To learn more about pelvic organ prolapse, please see here.
Otherwise, let’s jump into your questions!
Your POP & Tampons FAQS Answered
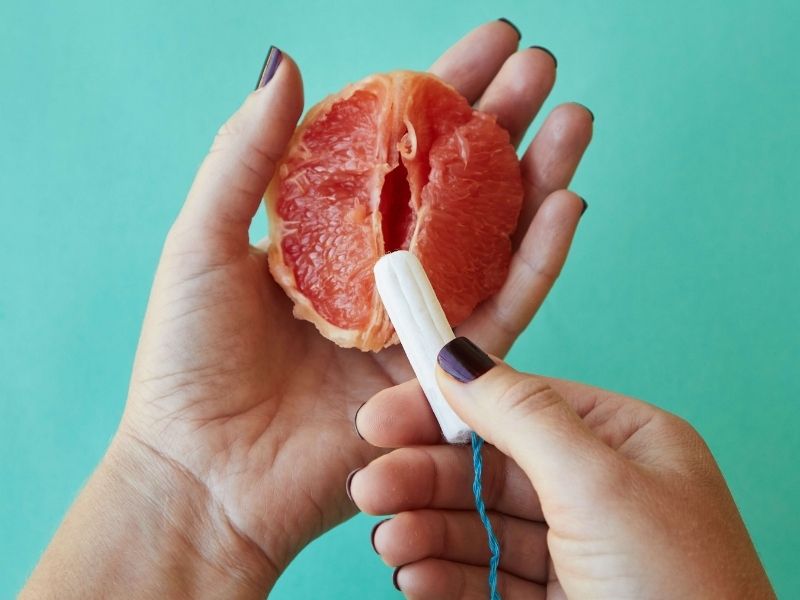
Can you use tampons with POP?
Your ability to wear tampons will depend on the nature and severity of your POP. You may not be able to wear a tampon if your cervix has fallen into your vagina. Women whose pelvic organ prolapse involves vaginal prolapse may find it difficult to use tampons.3 The best tampons with prolapsed uterus are those that feel comfortable for you.
Can you use tampons with a prolapsed uterus?
You may be able to use tampons if your uterus has prolapsed, but you may find it leads to irritation. If a prolapsed uterus or other organ leads to surgery for pelvic organ prolapse, then you cannot put anything in your vagina for six weeks after surgery—which means you can’t use a tampon for that time.4
Does wearing a tampon help with incontinence?
Some women take matters into their own hands and wear a tampon to help with mild prolapse and bladder leakage. While you may find this helpful, this is not a solution. Tampons are designed to absorb fluid and should only be used when you are on your period, according to their instructions. Wearing them to treat POP can lead to toxic shock syndrome.
Repeat: do not wear tampons to treat incontinence.
If you find that when you wear tampons, you get some relief from incontinence and POP, then speak to your doctor. You may be a good candidate for a device called a pessary, which is similar to tampons but specifically designed for this use, or other devices such as urethral inserts.
Unfortunately, too many women suffer in silence from POP and other pelvic floor disorders. It’s always better to speak to a doctor about any of your concerns, since many pelvic floor disorders are treatable, but can get worse over time.
Can a tampon put pressure on your bladder? Can a tampon cause incontinence?
Some women will only experience bladder leakage when they are using a tampon or menstrual cup. In this case, the patient may have bladder prolapse, but also have incontinence that is unrelated to the prolapse. If a tampon relieves your prolapse, but you still have leakage, then you may have another issue that is causing incontinence.
In other words, tampons don’t cause incontinence, but they may reveal that you have incontinence and help you understand the root causes of it.As with any and all questions related to your pelvic health, they are often best addressed by a pelvic health specialist.
Hormonal Fluctuations During Menstruation
How do hormonal changes throughout my menstrual cycle affect prolapse symptoms?
Throughout your menstrual cycle, hormonal fluctuations can significantly impact the symptoms of pelvic organ prolapse (POP). During the first half of your cycle, estrogen levels rise, which may strengthen pelvic muscles and ligaments, potentially reducing the sensations or symptoms associated with POP. This period often leads to a temporary alleviation or lessening of prolapse discomfort.
Why do my prolapse symptoms seem worse after ovulation?
After ovulation, which marks the midpoint of your cycle, estrogen levels drop and progesterone levels rise in preparation for a possible pregnancy. This hormonal shift can cause the pelvic floor muscles and ligaments to relax, potentially exacerbating prolapse symptoms. Many individuals notice their prolapse feels more pronounced or uncomfortable during this phase, leading up to their menstrual period.
Is it normal for prolapse symptoms to fluctuate with my cycle?
Yes, it’s entirely normal for prolapse symptoms to fluctuate in response to the hormonal changes of your menstrual cycle. Understanding this pattern can help you anticipate changes in your symptoms and manage them more effectively. If you’re finding the fluctuations difficult to manage, or if the changes in your symptoms are significantly impacting your quality of life, consulting with a healthcare provider specialized in pelvic health is recommended.
Can anything be done to minimize the impact of hormonal fluctuations on prolapse symptoms?
While it’s challenging to completely mitigate the natural hormonal fluctuations of your menstrual cycle, certain strategies can help manage prolapse symptoms more effectively. Maintaining a routine of pelvic floor exercises can strengthen the pelvic area and provide more support to prolapsed organs. Additionally, lifestyle modifications, such as maintaining a healthy weight and avoiding activities that strain the pelvic floor, can help. For some, hormonal therapies may also be an option. Always consult with a healthcare provider to determine the best approach for your specific situation.
Exercising During Menstruation With a Prolapse
For women with prolapse, is it safe to perform pelvic floor exercises, like Kegels, during their period?
Absolutely, it’s safe and highly recommended for women with prolapse to continue their pelvic floor exercises during menstruation. These exercises, Kegels included, play a crucial role in managing prolapse symptoms. Regularly strengthening the pelvic floor can provide enhanced support to the pelvic organs, which might ease the symptoms of prolapse. Additionally, this practice can offer relief from menstrual discomfort commonly experienced during this time.
Can women with prolapse find relief from menstrual discomfort through pelvic floor exercises?
Yes, many women with prolapse report that pelvic floor exercises contribute positively to reducing menstrual discomfort. Engaging in such exercises boosts blood flow to the pelvic area and helps maintain the muscle tone, which can be particularly beneficial in lessening cramps and alleviating menstrual pain. This supportive approach not only aids in managing prolapse symptoms but also improves overall comfort during menstruation.
Using a Pessary During Menstruation
Can I continue using my pessary during my period?
Yes, you can use a pessary during menstruation. However, it’s important to maintain good hygiene by removing, cleaning, and reinserting your pessary daily during your period. This helps prevent any potential for infection and ensures the device functions optimally.
Do I need to change how I use my pessary during my period?
The fundamental use of your pessary doesn’t change during menstruation, but paying extra attention to cleanliness is crucial. If you experience discomfort or if your menstrual flow is particularly heavy, consult with your healthcare provider for personalized advice.
Period Product Alternatives for Those with Prolapse
What menstrual products are suitable for someone with prolapse?
If traditional tampons are uncomfortable, alternatives like period underwear or specially designed menstrual cups can be excellent choices. These products can provide secure, leak-proof protection without the discomfort that some experience with tampons. Period underwear is designed to absorb menstrual flow while being gentle on the prolapsed area, and certain menstrual cups offer designs that can accommodate a prolapsed uterus more comfortably.
How do I choose the right menstrual product for my prolapse?
Consider products that align with the severity of your prolapse and your personal comfort. For mild prolapse, a menstrual cup with a wider top may offer a secure fit. For more significant prolapse, period underwear provides a non-invasive way to manage menstruation. Trial and error with different products can help determine the best fit for your needs.
Navigating Periods with Prolapse
How can I manage my prolapse symptoms during my period?
Managing prolapse symptoms during menstruation involves several strategies:
- Monitor Symptoms: Keep track of any fluctuations in your prolapse symptoms throughout your cycle to anticipate and manage changes.
- Dietary Management: To prevent constipation, which can worsen prolapse symptoms, eat a fiber-rich diet and stay well-hydrated.
- Pelvic Floor Exercises: Continue with your pelvic floor exercises to maintain muscle strength and support for your pelvic organs.
- Choose Comfortable Menstrual Products: Select menstrual products that fit your comfort level and prolapse condition, like period underwear or suitable menstrual cups.
What should I do if my prolapse symptoms worsen during my period?
If your symptoms significantly worsen during menstruation, consult with your healthcare provider. They may offer additional strategies or adjustments to your current management plan to better accommodate the symptomatic changes associated with your menstrual cycle.
Use our Physician Finder to locate one near you, and be sure to follow us on Instagram for regular tips to help support your pelvic floor health.