Endometriosis is a condition that impacts over 6.5 million women in the US alone, but it can still feel mysterious and hard to diagnose. Our team of medical experts are sharing all about endometriosis, and helping us all understand this common reproductive health issue!
What is endometriosis?
Endometriosis is a uncurable, but common pelvic health disorder categorized as Dysmenorrhea, a category of referring to monthly periods that cause women pain. It is named after being an abnormal condition of the endometrium, the inner lining of the uterus.
The endometrium is a crucial part of pregnancy; it is one of the few organs that has the ability to increase and decrease in size monthly. Every month, during a menstrual cycle, your body prepares for an embryo by releasing hormones to mature an egg in your ovary preparing it for insemination by sperm. These hormones also make your endometrium thicker, making it an ideal place for fertilization along with the nutrients needed for pregnancy.
If the egg is not fertilized by the male’s sperm, the body sheds the endometrium lining of the uterus, including the egg, which results in the bleeding or your “period”. For most women, this process continues monthly throughout her reproductive years without issue, but for 1 in 10 women endometriosis develops, usually diagnosed in their 30s and 40s.1
How do you get endometriosis?
Endometriosis refers to when endometrial-like tissue grows in sites other than the uterus lining. Over time, it may begin to grow usually on reproductive organs, like the ovaries or fallopian tubes, or within the abdominal cavity. There is no known cause for why this happens or how it can be prevented.
Despite growing outside the uterus, this tissue will continue to respond to monthly hormones and follow your menstrual cycle, increasing in size and breaking down each month. However, unlike your when you have your period, this tissue has nowhere to be discarded and exit your body. This can result in small amounts of bleeding inside of the pelvic area. Bleeding can lead to inflammation and swelling and eventually scarring of the normal tissue where the tissue is growing. 2
What are the first signs of endometriosis?
Early signs and symptoms may be difficult to identify as women exhibit varying levels of symptoms depending on the location of where the condition is developing and its severity.
However, the most identifiable symptom of endometriosis is pelvic pain, which will coincide with your period. As the endometrial tissue on your ovaries, fallopian tubes or other areas expands along with the endometrial tissue on the lining of your uterus. This expansion can create cramps characteristic of traditional menstrual pain, but more intense. This pain can continue to get more severe over time. 3
Having severe pain may not be indicative of the seriousness of your endometriosis. You could have a moderate case while experiencing severe pain or little pain with an advanced case4. Therefore, you should consult with a physician once you begin to feel pelvic pain. Endometriosis can be challenging to manage, the sooner you can be diagnosed the better a plan can be put into place to address your symptoms.
What does endometriosis feel like?
To best identify your symptoms, here are someone common signs and how the pain is often described5:
| Type of Pain | Symptoms |
| Pelvic | This will usually begin before your period and, typically, not manageable with pain medication. Discomfort can range from mildly irritating aches to strong, stabbing pains; your belly and pelvic area may feel as if they are being tugged on or have an extreme stiffening or burning sensation. |
| Back | Back pain is common symptoms you may experience as tissue from the uterus or ovaries can adhere to your lower back muscles. The pain will be felt more when you stand or make wide ranged motions involving your back muscles like stretching, yoga or chiropractor adjustments. |
| Leg | The sciatic nerve begins in the lower back and runs through the back of the thigh and leg to the foot. Tissue that builds on or around the sciatic nerve can create leg pain strong enough to makes it difficult for you to walk or stand up normally. You may notice cramps, pulsating pains, or stabbing pain in your legs. |
| Bowels | Tissue adheres to the rectum, vagina, and the tissues between which can result painful bowel movements. Women can experience irritable bowels, diarrhea and pain, or even constipation. They may also experience a tough time urinating and rectal bleeding. |
| Sexual | Tissues can develop into painful nodules in the uterus, cervix, or pelvic cavities that are felt as sharp pains during intercourse. The pain may be felt during sex or up to a few days following. |
For information on other symptoms disorders and their symptoms that may cause painful menstruation check out our post. Understanding Abnormal Menstruations
How to test for endometriosis?
Once you have spoken to a doctor or nurse about your symptoms, the location of where you are experiencing pain will be used to determine the next step of testing. Here are some of the most common diagnostic methods in order of least to move advanced6.
| Pelvic exam | Doctor feels for larger areas like cysts or scar tissue by using their fingers inside your vagina while pressing your abdomen. |
| Ultrasound | A handheld device is pressed against your abdomen or inserted into your vagina. This transducer creates images through sound waves of the inside of your uterus, most ideal for identifying the presence of large ovarian endometriomas (cysts)7. |
| Medicine | If ultrasound does not find signs of an ovarian cyst, hormonal medicine may be prescribed. If pain improves, you most likely have endometriosis. Once medication is stopped, pain is expected to return8. |
| MRI | You are placed inside a machine that uses radio waves and a large magnet to create images of your organs. This machine has a high detection of endometriomas, much better acutely than Ultrasound9. Its advantages allow doctors to determine your treatment plan, possibly without needing an invasive laparoscopy. |
| Laparoscopy | A surgical procedure performed by a surgeon, your doctor refers you to have a small incision (typically near your navel) where a small camera (laparoscope) is inserted to look for endometrial tissue or cysts that may have developed on your organs. A biopsy may be taken for testing.Often, the surgeon can fully treat endometriosis during the laparoscopy to avoid need for a second surgery. |
How to treat endometriosis10
There is no cure, but symptoms can be treated. Your doctor will recommend one of the following options, depending on severity.
| Medicine – Over the Counter Nonsteroidal anti-inflammatory drugs (NSAIDs), ibuprofen (Like Advil, Motrin IB) or naproxen sodium (Aleve) to help ease painful menstrual cramps |
| Medicine- Hormone Therapy Hormone medication may shrink existing endometrial tissue, slow or prevent new tissue growth, it will not eliminate existing tissue. |
| Hormonal contraceptives. Birth control pills, patches and vaginal rings may lightens and shorten menstrual flow potentially reducing or eliminating pain |
| Gonadotropin-releasing hormone (Gn-RH) agonists. Block the hormones that stimulate the ovaries to lower the amount of estrogen to prevent menstruation. Endometrial tissue should reduce in size. Other side effects, such as hot flashes, vaginal dryness and bone loss common during menopause may also decrease. |
| Progestin therapy. Progestins thin the lining of the uterus which stops regular periods and lessens the chance of bleeding works similarly on endometriosis lesions11. Delivered through an intrauterine device (IUD) with levonorgestrel (Mirena, Skyla), contraceptive implant (Nexplanon), contraceptive injection (Depo-Provera) or progestin pill (Camila). These therapies stop periods and the growth of endometrial implants, lessening endometriosis signs and symptoms. |
| Aromatase inhibitors. Lower estrogen levels in the body by stopping hormones from turning into estrogen, reducing the overall amount of estrogen in your body. These inhibitors may be prescribed with a progestin or hormonal contraceptives. |
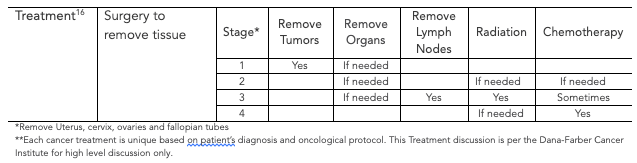
| Surgery. Surgery is only chosen when symptoms are serious and hormones are not providing relief. It may also be chosen if you are having fertility problems or trying to become pregnant. This will be performed laparoscopically ( the same as the test mentioned previously) and the endometrial tissue is removed. |
Is endometriosis cancer?
It is easy to see why Endometriosis could be a concern of uterine cancer, both involve abnormal growth of cells and tissues in the pelvic region and they share the most common symptom: vaginal bleeding. Bleeding is present in 90% of women at the time of their cancer diagnosis12. Nevertheless, research has not proven a connection between endometriosis and most types of gynecological cancer13.
Here are some important facts about endometriosis and uterine cancer:
Is endometriosis an autoimmune disease?
Your body has a natural defense system to fight against foreign cells that can make you sick. When your body is unable to tell the difference between your cells and foreign cells, it begins to attack your good cells. This is an autoimmune disease.
While endometriosis is not itself an autoimmune disease, studies suggest that it may put women at a higher risk of several autoimmune diseases, such as lupus, multiple sclerosis, rheumatoid arthritis and inflammatory bowel diseases (IBS)17. This may be due to women having endometriosis possibly having abnormal immune system responses18. Inflammation plays a role in the pain and other symptoms associated with these conditions, as it does with endometriosis, contacting a physician early when you may have symptoms may help you get ahead of diagnosis and treatments for these autoimmune diseases.
Is endometriosis hereditary?
Some studies have suggested that women whose family members have endometriosis are more likely to develop the disease. While most doctors believe all women will experience some type of endometrial tissue, it is the women with immune problems that will develop endometriosis.
There is some belief that there may be a birth defect that develops endometrial cells outside of the uterus when the fetus is growing. Then, when this female matures to start menstruation, these cells develop into the tissue that enlarges with the release of monthly hormones, causing pain and discomfort19.
Can you get pregnant with endometriosis?
Pregnancy is possible if diagnosed, but treatment is recommended to increase your chances. A study found that when looking at couples trying to get pregnant on a monthly basis that 15-20% of the couples will be successful, that number drops to 2-10% if suffering from endometriosis20.
This endometrial tissues that is growing out of the uterus lining can damage or even prevent the reproductive organs from performing their functions, making it more difficult to get or even stay pregnant, carrying a baby to full term.
Laparoscopic surgery will most likely be used remove the extra tissue to improve your fertility and chance of getting pregnant.
Having endometriosis is common and is quite manageable. If you are noticing monthly periods are becoming more painful than normal or feel you are experiencing other unusual symptoms in your pelvic area, let your physician know. The earlier the diagnosis, the better the prognosis to return you back to your normal pelvic health.




















